By Javier Fernández Ruiz

Javier Fernández Ruiz holds a PhD in Biology (1986) from the Complutense University of Madrid (UCM). He is currently a professor in the UCM's School of Medicine. He has been working as a researcher for the last 36 years and has written many research articles and chapters for books. He has filed 5 patents. He lectures in universities, research centres and at conferences. He is currently the principal investigator of the CANNABINOIDS-BBM3 research group of the University Institute of Research in Neurochemistry at the UCM, the CIBERNED, and the IRYCIS. The group's work centres on the study of the therapeutic potential of cannabinoids in various neurodegenerative diseases. It collaborates with several Spanish and international groups. Dr Fernández Ruiz has been principal investigator on 26 research projects. He was the president of the "International Cannabinoid Research Society (ICRS)" from 2002-2003 and was a founding member of the Spanish Cannabinoid Research Society (SEIC), of which he has been the Secretary (2000-2007) and President (2007-2011). He currently sits on the governing board of the IRYCIS, the scientific advisory board of the company VivaCell Biotechnology Spain and the editorial committee of the British Journal of Pharmacology.
The biomedical challenge of neurodegenerative disorders in XXI century
Epidemiological data indicate that the incidence of neurodegenerative disorders in the World has experienced a significant elevation in the past 30 years. Such elevation is the result of a simple fact: the increased longevity, particularly evident in developed countries, which gives neurodegenerative disorders more opportunities to be visible.
The case of Spain faithfully reflects the reason of this problem. Our life span is presently close to 90 years in the case of women and around 85 years in the case of men, and, given that the incidence of Alzheimer's disease is approximately 9-fold higher in individuals of 85-89 years (20.1%) compared to subjects 20 years younger (2.2%), with similar numbers in Parkinson's disease, Huntington's chorea or other neurodegenerative disorders, the conclusion is clear: living longer means more possibilities to suffer one of these disorders. The current situation already represents a great biomedical issue, which will be aggravated in coming years, as the expectation of a 2-fold increase in the world population for 2030, with greater percentages of people over 65 years old compared to younger ages, will mean to multiply by 2.5 the incidence of Parkinson's disease in China, by 2.1 in India and Brazil, by 1.9 in USA and by 1.5 in European countries, with similar numbers for other neurodegenerative disorders. The major problem is that we are not prepared yet for such biomedical challenge, as the progress in therapies useful to treat symptoms of these diseases and, in particular, to delay, arrest or repair the neurodegenerative process, is still limited. The question is that the generation of neuroprotective therapies has been an important research objective for years, with numerous antioxidant, anti-inflammatory or antiexcitotoxic agents, apoptosis inhibitors, autophagy enhancers, neurotrophic factors, and other types of compounds extensively investigated for their ability to preserve, rescue and repair neurons. However, the testing of these compounds was failed directly in cellular or animal models, or at the time of reproducing in humans the positive effects found in the experimental models. To identify the causes for these permanent failures is a key but still unsolved question. Several aspects appear to be particularly important, for example, the need to work with compounds having a broad-spectrum profile. Present investigated neuroprotective strategies are addressed to limit only one of the different mechanisms leading to neuronal death, for example, limiting excitotoxicity, oxidative stress or inflammation, or enhancing autophagy or neurotrophic support. It is evident today that neurotoxic events cooperate each other to kill neurons and glial cells in neurodegenerative disorders, so that any effective neuroprotective therapy should be necessarily developed following a polypharmacology strategy, namely broad-spectrum agents capable to limit most, if not all, of the different cytotoxic events at the same time, or using combinations of more selective agents. In addition to the use of neuroprotective agents, it is also necessary to develop neurorepair strategies to restore the loss of neurons. The clinical diagnosis of most of neurodegenerative disorders, particular if they have sporadic origin, frequently occurs when first neurological symptoms appear, and, at these stages, neuronal losses are already important. In this situation, the treatment should attempt not only to preserve the surviving neurons, but also to replace those lost during the presymptomatic phases of the disease. Associated with this last question, it is also important to progress in the identification of early biomarkers that, during such presymptomatic phases, may already alert on the existence of the disease, despite the absence of diagnosed clinical symptoms. For example, individuals in risk of progressing towards the symptomatic phase of Alzheimer's disease might be earlier detected measuring biomarkers based on neurological recording (e.g. evidence of mild cognitive impairment), imaging techniques (e.g. PET to detect early β-amyloid aggregation or signs of synaptic dysfunction; volumetric MRI to detect brain structural changes), or biochemical analysis in biological fluids (e.g. tau levels in the CSF). With such early diagnosis, neuroprotective treatments might be initiated before the extent of brain damage is large, then enhancing the possibilities of having positive results in clinical trials.
Cannabinoids as a promising neuroprotective/neurorepair therapy
Cannabinoids, including plant-derived, endogenous and synthetic compounds, has been investigated during the last 10-15 years because they may preserve neurons and also glial cells (e.g. astrocytes, oligodendrocytes and their precursor cells) against numerous types of insults that impair cell homeostasis and integrity. Such cytoprotective properties have attracted the interest for developing cannabinoid formulations, also including medicinal cannabis, to be investigated first in preclinical models of specific neurodegenerative disorders and eventually used in clinical trials with patients suffering of Alzheimer's disease, Parkinson's disease, amyotrophic lateral sclerosis, Huntington's chorea and other important chronic neurodegenerative disorders. They are also under investigation in acute brain damage, e.g. stroke, brain trauma, spinal injury. The way towards having licenced cannabinoid-based medicines for these disorders will be still long, but modulating the multiple targets for the neuroprotective properties of cannabinoids offers important advantages over previously investigated neuroprotective agents. It will be necessary to identify the best targets and to strengthen the preclinical evidence, as well as to optimize cannabinoid-based treatments for each disorder, but the hope recruited by cannabinoid formulations deserves to move the issue towards the clinical scenario.
The first advantage of cannabinoids as neuroprotectant agents is their broad-spectrum action. In general, they have a relatively similar potency compared to classic antioxidants, antiglutamatergic or anti-inflammatory agents investigated for their neuroprotective properties, this is not the added-value. The advantage is that they may recruit in a single molecule, or in a combination of two or more cannabinoids, capabilities to be active against most of the harmful stimuli that damage neuronal homeostasis and integrity. This advantage is extremely important as excitotoxicity, inflammation, oxidative stress and other neurotoxic stimuli (e.g. mitochondrial dysfunction, protein aggregation) work, as mentioned above, cooperatively to kill neurons. In such conditions, it is extremely difficult to limit neuronal damage with compounds or strategies having activity at only one of these cytotoxic events. An efficacious therapy would need, as mentioned above, the use of a "multi-target strategy" using the combination of different therapeutic agents. Such broad-spectrum strategy is something that cannabinoids may exert, given their capability to act at different molecular targets related to neuronal homeostasis and survival. Part of these targets belong to the endocannabinoid system, e.g. cannabinoid receptors, or endocannabinoid enzymes, which may be activated or inhibited with the result of neuroprotection, but additional targets, even outside the endocannabinoid system, are also available for neuroprotective cannabinoids. In addition, cannabinoids, in particular plant-derived cannabinoids, have a recognized antioxidant profile, which would be receptor-independent and based on their ability to act as scavenger of reactive oxygen species. Such antioxidant profile was the first neuroprotective action that was investigated for this family of compounds (see attached figure).
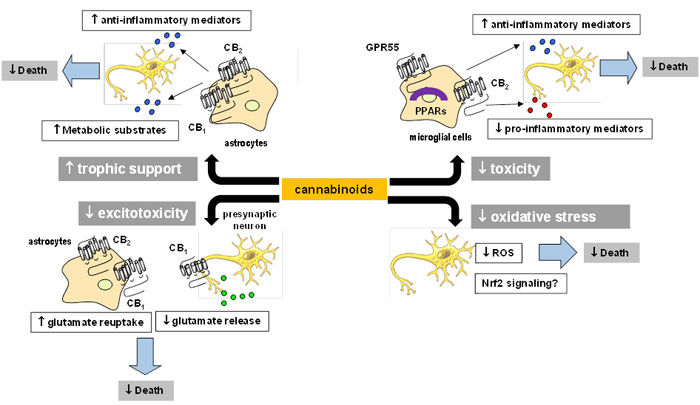
The broad-spectrum neuroprotective profile of cannabinoids is the consequence of singular anatomical circumstances: that molecular targets available for cannabinoids to exert their neuroprotective effects are located in cell substrates, which play key roles in the processes of degeneration, protection, repair and/or replacement. This singular circumstance again represents an important advantage for cannabinoids compared to classic neuroprotectants. For example, the control exerted by cannabinoids on excitotoxic damage is facilitated by CB1 receptors that are located in neuronal sites, in particular in glutamatergic neurons, in which their activation with cannabinoids inhibits the excessive glutamate release which is toxic for neurons. This benefit derives from a key location of CB1 receptors in glutamatergic synapses (see attached figure), but sums to other benefits derived from the presence of these receptors in non-neuronal cells such as astroglial cells located in the vicinity of glutamatergic synapses. The activation of astroglial CB1 receptors, alone or in combination with CB2 receptors, may also contribute to reduce the toxicity of glutamate by promoting its clearance from the synapse through classic astroglial glutamate transporters (see attached figure).
Astroglial CB1 and CB2 receptors may also work in a concerted manner to regulate other astrocyte functions that are relevant for neuronal homeostasis and integrity, for example, to improve the trophic role exerted by these glial cells for neurons. This includes to promote the supply of metabolic substrates, as well as the generation of neurotrophins, anti-inflammatory mediators or prosurvival factors, which could potentially rescue damaged neurons (see attached figure). A third important cell substrate containing neuroprotective targets for cannabinoids is microglial cells, in particular when they become reactive, a condition in which the levels of CB2 receptors are strongly elevated. Such elevation has been associated with the role of these receptors in the proliferation and migration of these cells at lesion sites, as well as with an attempt to limit their toxicity by inhibiting the plethora of pro-inflammatory mediators generated by these cells with capability to damage neurons. By activating microglial CB2 receptors, cannabinoids are able to limit microglial toxicity, an effect that cannabinoids may also produce by activating additional molecular targets such as the orphan receptor GPR55 or the nuclear receptor PPAR-γ (see attached figure). CB2 receptors have been also identified in a third type of non-neuronal glial cell, oligodendrocytes, as well as in their precursor cells. In these cells, the activation of this receptor contributes to their key function, which is the formation of myelin, something that is essential in demyelinating disorders like multiple sclerosis. Again, this is a crucial event for neurons facilitated by the location of molecular targets for cannabinoids in those cells responsible of such event.
Another relevant discovery in relation with the importance of cannabinoids in neurodegenerative disorders is related to the presence of CB2 receptors, and also CB1 receptors and other endocannabinoid elements, in neural progenitor cells. These cells are essential for the natural replacement of neurons and glial cells which are deteriorated and need to be replaced during life. Our present knowledge on the processes of cell replacement in the adult brain is still limited, but, contrarily to former ideas on the absence of neurogenic processes in the adult brain, today it is evident that certain areas of the human brain have capability to generate new cells, in particular new neurons. Cannabinoids, by acting on specific molecular targets located in neural progenitor cells, may promote the processes of proliferation, maturation and/or differentiation of these precursor cells, and this represents a relevant advantage that enable cannabinoids to provide not only neuronal protection, but also neuronal repair and replacement, something critical in disorders in which the diagnosis occurs when the neuronal damage has progressed significantly.
Therefore, three important advantages, namely their broad-spectrum neuroprotective profile and their neurorepair capability, which found explanation in the location of their molecular targets in key cellular substrates for cell survival, situate cannabinoids in a promising position to serve as novel neuroprotective/neurorepair agents in neurodegenerative disorders. As a final conclusion, it is important to remark that these neuroprotective/neurorepair properties exerted by cannabinoids appear to be simply the natural consequence of the pharmacological reproduction of an endogenous protective response exerted by the endocannabinoid system (which contains most of the molecular targets that are activated by cannabinoids) against neurotoxic (inflammatory, excitototoxic, traumatic, oxidant) stimuli that may damage the brain. The idea of the endocannabinoid system as an endogenous protective system has been formulated to explain the responses against brain damage experienced by specific elements of this signalling system, in particular the elevated generation of endocannabinoids and the induction of CB2 receptors in glial cells. If this is correct, the pharmacological activation of these elements with cannabinoids would be simply a useful way to enhance the endocannabinoid elevation and their subsequent cannabinoid receptor activation, mainly the CB2 receptor, typically found in neurodegenerative conditions. The present research in this field is addressed to progress in the knowledge of this key function of the endocannabinoid system, and to ensure that this work derives in the development of efficacious neuroprotective/neurorepair therapies that may reach the clinical scenario.