By Manuel Guzmán

Manuel Guzmán is Professor of Biochemistry and Molecular Biology at Complutense University of Madrid, member of the Spanish Royal Academy of Pharmacy, and member of the Board of Directors of the International Association for Cannabinoid Medicines. His research focuses on the study of the mechanism of action and therapeutic properties of cannabinoids, especially in the nervous system. This work has given rise to more than one hundred publications in specialized international journals, as well as to several international patents on the possible therapeutic applications of cannabinoids as anticancer and neuroprotective drugs. He routinely collaborates with scientific reviewing and funding agencies.
In recent decades, a large number of studies has accumulated showing that cannabinoids (and especially the main active component of cannabis, Δ9-tetrahydrocannabinol, or THC), exert anti-tumour effects in mouse and rat models of cancer. Therefore, it is now well-established that the administration of cannabinoids to such animals can reduce the growth of different types of tumour cells, including brain, skin, lung, breast, pancreatic, liver, prostate and others.
This research has also provided insight into the mechanisms by which cannabinoids mediate their anti-tumour effects through CB1 and CB2 receptors located on the surface of tumour cells. For example, cannabinoids are able to (a) inhibit proliferation, (b) cause death and (c) prevent the migration and invasion of tumour cells. These, let's say "classic", anti-tumour effects of cannabinoids have already been reported in several articles published on the Fundación CANNA website by some of my colleagues (Guillermo Velasco, Cristina Sánchez, Mariano García de Palau, Saoirse O'Sullivan and Mike Tagen — I apologise if I have forgotten anyone) and myself. Since these effects are observed not only in experimental animals, but also in tumour cells grown in isolation in Petri dishes, it is assumed that cannabinoids exert these effects directly on tumour cells. Or, to use the jargon of cell biology, they are "autonomous" from tumour cells.
However, it is obvious that, in a tumour, tumour cells are not alone and that they establish both physical and chemical connections with other neighbouring cells, such as those of the extracellular matrix (fibroblasts), those of the immune system (leukocytes such as T-lymphocytes and macrophages), and those of blood vessels (the myocytes of the muscular wall and endothelial cells of the inside of the vessels). Indeed, the mechanisms by which these non-tumour cells can indirectly affect the growth of malignant cells are increasingly understood, and on this basis, therapies (especially immunotherapy) have been designed to prevent tumour growth by targeting non-tumour cells. In this case, following the above jargon, we are talking about processes of the tumour cells that are "non-autonomous". Turning to cannabinoids, very little is known about their "non-autonomous" anti-tumour effects, i.e. how they affect communication between tumour and non-tumour cells.
Let us focus on the brain, the organ in which the anti-tumour action of cannabinoids has mostly been studied. Our group has long shown that cannabinoids can help block the growth of brain tumours in mice by inhibiting angiogenesis, the process by which the tumour manages to generate its own network of blood vessels, so that it can, for example, more easily obtain the nutrients and oxygen it needs to grow, as well as excrete the waste products resulting from its high metabolic rate. Specifically, these studies showed that cannabinoids inhibit the production of one of the main proteins involved in tumour angiogenesis (vascular endothelial growth factor, or VEGF), leading to a reduction in the number and size of tumour vessels. However, until now it was not known whether cannabinoids in the brain can affect the interaction of tumour cells with the main non-tumour cells, i.e. neurons. This has been the focus of a recent study* that our group has carried out with the generous sponsorship of the Fundación CANNA, which I will summarise below.
To try to answer this question, we used melanoma as an experimental model. This is a tumour that primarily affects pigmented skin cells (melanocytes) and is one of the most malignant types of cancer, especially due to its high capacity to metastasise to various organs, including the brain. In practice, it is estimated that more than 90% of patients with melanoma brain metastases have a life expectancy below 3 years from diagnosis. Understanding the molecular mechanisms that control the brain metastases of melanoma is therefore of paramount importance to try to design new targeted therapies for this devastating disease. From a biochemical point of view, our focus was on glutamate, the main excitatory neurotransmitter produced by our brain, as there was previous evidence that this molecule can interact with some tumour cells and facilitate their proliferation.
First, we performed computational studies (in silico studies) on publicly available databases containing molecular information on many thousands of tumour biopsies from cancer patients. Specifically, when we analysed data from melanoma samples, we observed that they contained abnormally high levels of glutamate receptors, which would logically allow melanoma cells to recognise and eventually respond to glutamate.
Secondly, we undertook studies with melanoma cells isolated and cultured in Petri dishes (in vitro studies). When we used specific blocking molecules to stop the action of glutamate receptors (and in particular a specific subtype, the so-called "NMDA receptors"), we saw that melanoma cell proliferation was indeed prevented.
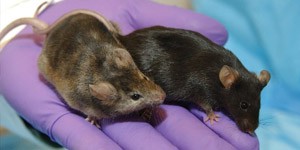
Thirdly, we conducted studies in mice bearing melanoma metastases in the brain (in vivo studies). The CB1 cannabinoid receptor located on glutamate-synthesising neurons (the so-called "glutamatergic neurons") is known to prevent the release of glutamate into the extracellular environment. We observed that this CB1 receptor present in glutamatergic neurons blocked glutamate access to neighbouring melanoma metastases, thus preventing their proliferation. As a control for the specificity of this effect, we showed that the CB1 receptor located on different, non-glutamatergic neurons did not affect the proliferation of melanoma brain metastases.
In summary, this work reinforces the idea that the anti-tumour effects of cannabinoids in the brain are not only due to direct ("autonomous") actions on tumour cells, but also to indirect ("non-autonomous") actions exerted on other cell types (in this case, glutamatergic neurons).
More broadly, the study reveals a new molecular mechanism involved in the growth of melanoma brain metastases, which could, perhaps, contribute to the design of antineoplastic therapies based on the inhibition of the action of glutamate.
*Original article:
Costas-Insua, C., Seijo-Vila, M., Blázquez, C., Blasco-Benito, S., Rodríguez-Baena, F.J, Marsicano, G., Pérez-Gómez, E., Sánchez, C., Sánchez-Laorden, B. & Guzmán, M. (2023) Neuronal cannabinoid CB1 receptors suppress the growth of melanoma brain metastases by inhibiting glutamatergic signalling. Cancers 15, 2439.