By Yuval (Tuby) Zolotov

Yuval (Tuby) Zolotov is a medical cannabis researcher and a PhD student at the School of Public Health at the University of Haifa. He completed his Master in Health Administration at Bar Ilan University where he investigated adherence to medical cannabis among licensed patients in Israel. Before joining academia in 2012, Yuval was a licensed Patient Instructor and has been involved with the local industry since its inception. While working on his thesis – Medical Cannabis Recommendation: Understanding and Predicting Physicians’ Behavior – Yuval is also involved in various research projects.
Meet the Experts is a series of interviews conducted by experts from the field of Cannabis to world leaders in research and clinical practice of Cannabis as medicine.
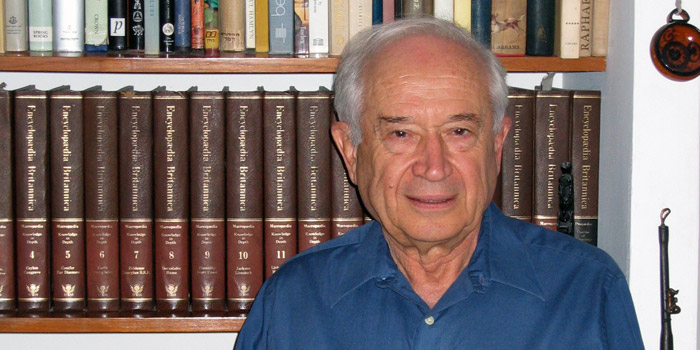
Raphael Mechoulam is a professor of medicinal chemistry at the Hebrew University of Jerusalem (Israel). During his many years of a fruitful scientific work, he has contributed significantly to the science of cannabinoids and the endocannabinoid system as we know it today. Among those unprecedented contributions are the isolation and synthesis of THC (in collaboration with Prof. Gaoni) and the identification of the endocannabinoid system. His work has awarded him with many honors and awards, including the Israel Prize (2000), NIDA Discovery Award (2011) and many others.
Yuval Zolotov: Your work has contributed significantly to the development of medical cannabis in recent decades. What is your opinion on where we stand these days?
Raphael Mechoulam: I am optimistic. In general, I think that we are moving in the right direction, and there are constantly new developments which allow more patients access to medicinal cannabis. The situation obviously differs greatly from one place to another, so there is quite a lot of variability in this sense. I am most familiar with the Israeli regulations, and I also serve as an advisor to the Israeli Ministry of Health. I think that in Israel we have come relatively far because the Ministry of Health has acknowledged that cannabis may be helpful for certain conditions. And that is a good starting point. Although the regulations are a work-in-progress, the fact that more and more patients are licensed may serve to prove that we have already achieved some progress. Currently, physicians can recommend medical cannabis for patients who suffer from a symptom or a disease that is included on the list of approved indications; the Ministry of Health regularly reviews this list, and cautiously considers including more diseases, mainly ones with mental symptoms. So there is still a way to go – because according to previous studies, some of which I contributed to, it is plausible that other patients may benefit medically from using cannabis.
YZ: What do you think is obstructing progress?
RM: There are still quite a few problems. I am a chemist, and so my point of view is exclusively scientific. From a chemist's perspective, there is no such thing as "medical cannabis", because this is something that is not standardized. It is not a medicine. We need to have very well defined products so we can specify which cannabinoids are better for which indications, and what the right dosages are, and side effects of course. I believe this is the only way to allow more patients to benefit medically from cannabis. We already know that THC and CBD have different properties. We also know that sativa strains differ from indica strains. In Israel, instead of having a variety of strains, the regulatory plan is to have just a few types of cannabis that will be standardized more strictly. The current standardization does not match the medical standards closely enough. And the strains that licensed growers are currently dispensing to patients are not typified or standardized enough. And most of them have weird names, by the way.
YZ: What other concerns do you have aside from standardization?
RM: There is a lack of clinical research, and that is the other side of the same coin. The regulations are still restricting research on cannabis. More and more evidence is accumulating, but certainly not enough yet. So many cancer patients around the world have used cannabis for years, but still there is not even one randomized-controlled clinical trial with cancer patients. Every medication goes through clinical trials. And clinical trials cost money, usually quite a lot. The funding is another big issue. Clinical trials are usually funded by pharmaceutical companies, but it seems that those companies are not interested in investing in cannabis. Since it cannot be patented, they would probably not get a return on their money. Hopefully, governments should be interested in this kind of data, but we know that governments, in general, don’t have the capacity needed to do such research.
YZ: How do you think more such trials can be promoted?
RM: I know I am being interviewed, but I don’t have all the answers. Clinicians in Israel, whom I collaborate with, have found ways to facilitate studies; some received grants, donations or other contributions. Thus, there are already more clinical trials that are currently in progress. For example, a preliminary study on CBD for the prevention and treatment of GvHD1 had very good results, and now they are doing the second trial with more patients. So in the future I see no reason for cannabidiol not being a first-line treatment for GvHD. And this is only one example, and it is quite exciting actually. There is still a long way to go, but I feel that we are going in the right direction.
YZ: When you say that cannabidiol might be a treatment in the future, do you mean herbal canabidiol or a synthetic one?
RM: As a chemist, for me cannabidiol is a defined substance, and its origin shouldn’t matter. Whether it is derived from herbal cannabis or synthetic – they should be the same compound. In the lab, cannabidiol is easy to work with, and it can be isolated from herbal cannabis to a level of total purity. But it might as well be synthetic.
YZ: Other than THC and CBD, which other cannabinoids do you think should be studied more thoroughly?
RM: It may very well be that other cannabinoids can provide therapeutic benefits. I also think there should be more focus on the acidic precursors of THC and CBD – THCa and CBDa. Those molecules have low stability, and as a result, very little research has been done on them. But I think that they have a big potential and should be studied more.
YZ: How do you see the situation 5 years from now? And 10 years from now?
RM: I think that the products will be better analyzed and standardized, and hopefully there will be more clinical evidence. We will know more about the "entourage effect". But if we look at the pharmaceutical markets and how medications evolve, I also think that the situation will be very different than it is today. We cannot use penicillin, but only derivatives of it. It may take more than 5 years, but the situation will probably be the same with cannabinoids. Concurrent with the expanding use of medical cannabis, I believe there will be more semi-synthetic derivatives, mainly of CBD, but also of THC. In addition, I expect that once we acquire more knowledge, we can treat more patients with different kinds of medical conditions, greater numbers than today. For instance, there are 80 auto-immune diseases, in which the body attacks itself. Based on studies in the lab, mine and others, it is plausible that cannabidiol can treat at least some of them. So there is lots to do.
YZ: Do you think that cannabinoids should also be used for the treatment of mental illnesses?
RM: This is a much more controversial topic. Based on some evidence, it may help several mental conditions, such as schizophrenia. Currently, post-traumatic stress is the only mental indication that is eligible for medical cannabis according to the Israeli regulations. We did a small study with human subjects which had very good results. But the government is very careful about approving new mental indications. There are many concerns that people would fabricate a medical problem to try to take advantage of the regulations, and mental illnesses are much easier to fabricate.
YZ: What is your opinion on recreational use and the legalization of cannabis?
RM: In my opinion, the discussions about the medical use of cannabis and about its recreational use should be completely separate. One really has nothing to do with the other. Medical cannabis needs to adhere to strict medical standards, and this is still not the case as I mentioned. The recreational use of cannabis is a societal matter, so society has to decide about it. It's not involved with medical considerations. Some people do use the medical properties of cannabis as a rational basis for advocating recreational use. I don’t think that is relevant at all. Alcohol may be dangerous, but societies have decided that it is legal. It is believed that life expectancy is lowered by a high consumption of alcohol, but I haven’t heard that they are considering making it illegal. So those questions are beyond the medical perspective. My interest and my work through the years have focused solely on the medical aspects. The medicinal potential of cannabis is huge, and we should not miss out. I believe that this potential is no longer being ignored, and that's why I'm satisfied with the recent developments of medical cannabis policies. I think that in the future, more and more patients will have access to medical products based on cannabis and cannabinoids. Science will continue to accumulate data, and we will know more. While the use of medical cannabis is undoubtedly going to expand, my hope is that it will do so in a rational way.
YZ: Thank you very much for granting us this interview.
1. Graft versus host disease (GvHD) is a medical condition which can develop after a bone-marrow transplantation, in which the donated bone marrow attacks the recipient-patient's body (Y.Z).


