By Kyle Boyar

Kyle Boyar is a cannabis scientist with a background in neurobiology and analytical chemistry who has been working in the industry for six years. Kyle received his Bachelor's degree in Neuroscience from the University of California Santa Cruz and was previously employed as a Laboratory Manager for SC Laboratories. Kyle is currently employed as a Field Application Scientist with Medicinal Genomics where he assists cannabis testing labs and growers with testing for microbial contaminants, plant pathogens, and genetic traits. In addition to his work with Medicinal Genomics he also serves as the Scholarship Committee Chair and Social Media Coordinator for the American Chemical Society's Cannabis Chemistry Subdivision.
According to the United Nations, 158.8 million people around the world use cannabis – more than 3.8% of the world's population. Cannabis can be administered through a variety of means such as inhalation, oral ingestion, or topical application, just to name a few.
Each product and unique route of administration presents its own microbiological considerations. This is partially why third-party safety testing has become a mandated in both medical and recreational cannabis markets. In the context of microbiological testing, the cannabis industry has chosen to adopt methods commonly used in the food industry such as plating and culture-based systems. However, sequencing of the cannabis microbiome and analysis of the data produced by of many of these methods has shed light on various inefficiencies and pitfalls of commonly used practices and creates a strong argument for the use of molecular methods [1-2].
Why is microbial testing needed?
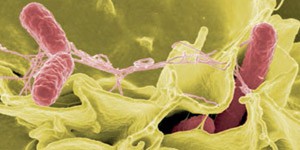
Microbial testing is essential to ensure that cannabis users are not being exposed to harmful contaminants. For healthy individuals some microbial contaminants are relatively harmless This is especially important for patients using cannabis to treat a condition as many of them have compromised immune systems making them particularly susceptible to contracting illnesses due to microbial contamination. The most prevalent risk for these patients is aspergillosis, a respiratory infection caused by the inhalation of Aspergillus spores that can be fatal if untreated. There are a handful of documented cases of this infection in immunocompromised patients that stem from the consumption of cannabis contaminated with spores of Aspergillus [3-15]. A recent case study showed that this infection is not always limited to the immune compromised and can even occur in healthy individuals [16]. There have also been documented cases of Salmonella outbreaks due to contaminated cannabis [17].
What kinds of microbial contaminants do labs test for?
In the absence of universal microbial requirements, it has mostly been in the hands of regulatory bodies as well as local and state jurisdictions to determine what types of contaminants cannabis testing labs should be screening for. Currently, many labs are performing total count tests that target large microbial groups that are considered indicator organisms such as: aerobic bacteria, coliforms, enterobacteriaceae, and yeast & mold. While these tests can provide information about the microbial load in a sample they cannot differentiate between harmful and benign microorganisms. Some states are aware of these drawbacks and have opted for species-specific testing for known human pathogens such as Salmonella, Shiga-toxin producing E. Coli (STEC), and certain species Aspergillus. These pathogen specific tests provide much more useful information in the context of consumer safety.
However, microbes themselves are not the only area of concern for cannabis users. Some fungal contaminants can also produce harmful secondary metabolites called mycotoxins. These compounds are highly toxic even at low levels and can lead to illness, disease, and in some cases can be fatal. For example, Aspergillus is a common contaminant found in cannabis and some species can produce mycotoxins such as aflatoxin and ochratoxin. These compounds are known mutagens and carcinogens that are toxic to the liver. DNA sequencing of cannabis microbiomes has also revealed additional organisms that could produce compounds of concern. Penicillium citrinum and Penicillium paxilli are fungi commonly found on cannabis that produce the mycotoxins citrinin and paxilline. These compounds block certain ion channels in the brain and could have serious implications for conditions like epilepsy. Specifically, paxilline has been shown to produce tremors and has been shown to attenuate the anti-seizure properties of CBD in mouse models [18]. Similarly, citrinin is another mycotoxin that disrupts certain mitochondrial pathways that CBD interacts with to provide seizure reduction [19]. Considering CBD is administered to achieve concentrations in the µM concentration and these toxins can have negative effects in the nM concentration the presence of these microbes in numerous cannabis samples is cause for concern. A few states have chosen to mandate testing for these fungal contaminants however it is not a universal testing requirement therefore many labs are not screening for them.
What are the commonly used methods for the microbial testing of cannabis?
One of the most commonly used culture-based methods in cannabis testing is 3M Petrifilm. These films are compact versions of a petri dishes that utilize selective antibiotic media and a specific readout chemistry that allows for the enumeration of certain microorganisms. Other culture-based methods being used in the cannabis testing field include Biomerieux's Tempo & Vidas as well as BioLumix, which also employ similar methods of detection for certain classes of microorganisms. There are also analytical chemistry-based methods such as matrix-assisted laser desorption ionization time-of-flight mass spectrometry (MALDI-TOF-MS) which is able to identify microbial contaminants at the broader class and subspecies level based on presence of certain macromolecules associated with a given microbe. This methodology is currently being used in the clinical world and offers a rapid method for microbial detection however the costs associated are quite high as these instruments can cost upwards of half a million dollars [20]. Alternatively, qPCR is a DNA-based molecular method that allows for the measurement of a DNA target associated with a given contaminant using a fluorescent reporter molecule. Due to lower instrumentation costs and increased sensitivity, qPCR is often the go to methodology for this kind of pathogen testing. When it comes to testing for mycotoxins produced by microbial contaminants liquid chromatography coupled with tandem mass spectrometry (LC-MS-MS) is generally the preferred methodology although other less sensitive methods do exist.
How do these methods differ from each other?
Comparing these methods is like apples and oranges for a number of reasons.
- 99% of microbes do not culture [21], therefore culture methods are only able to detect a small subset of microorganisms.
- The act of culturing changes microbial load – Because culturing essentially is providing a medium that fosters certain types of microbial growth some species are favored over others and outcompete other species. This produces a very different picture from what is initially present on the sample causing a distorted image of the microbial communities present on cannabis material or cannabis products.
- Differences in selectivity – Traditional plating methods typically rely on antibiotics for their selectivity while qPCR and MALDI-TOF-MS rely on target sequences or molecular signatures specific to the microorganism(s) of interest. These differences in selectivity can cause deviations in the results reported, especially when comparing to culture methods which have been shown to also grow off target organisms in some cases.
- Turn-around time can greatly vary with culture-based methods and can produce results as quickly as 24 hours or as long as ten days depending on the microorganisms of interest. Molecular methods like qPCR can provide same or next day results depending on if the organism of interest will require an enrichment.
- Culture-based methods will only grow viable cells while qPCR and MALDI-TOF-MS do not discriminate between live and dead organisms.
Considerations for the microbial testing of cannabis
The microbial testing of cannabis is complex due to many different variables some of which are unique to the plant. One of these unique properties is the microbial communities that are naturally reside in the plant. These endogenous microbes are called endophytes and act probiotics for the plant either by preventing the colonization of harmful microbes or by aiding in the production terpenes which serve as a defense mechanism against insects and other predators. Some of these microbes will grow in culture and cultivators often apply these beneficial microbes as foliar sprays which can lead to elevated counts when performing total count tests even though the product is perfectly safe for use.
There are also microbial contaminants in cannabis that can elude some methods. Unculturable microorganisms such as botrytis and cannabis derived powdery mildew are some examples of this. In addition to unculturable microbes, cannabis can also be contaminated with microorganisms like Ralstonia, which is a bacterial pathogen that lives inside of fungal cells many of which are common to cannabis. It is also a known cause of respiratory infections in immunodeficient populations [22-23]. Since these microorganisms are found inside of the cell culture methods will not pick up these contaminants.
Another issue that adds to these complexities is a lack of standardized methods for the microbial testing of cannabis flower and other cannabis products. Furthermore, many labs are utilizing microbial testing methods that are meant for food products and have not been validated on cannabis and other cannabis product matrices. This lack of validated methods for cannabis combined with differing methodologies between testing laboratories can cause large deviations in reporting from lab to lab.
Future Directions and Conclusions
Microbial testing for cannabis is complex due to the wide range of methodologies being used, the diverse matrices in which cannabis is delivered, and the unique microbial communities found on the plant. To address these obstacles, it is important for laboratories to develop and establish consensus methods for microbial testing. Regardless of which methodology is adopted, the lab employing the method should validate it internally on all matrices being tested to ensure optimal detection and/or quantification of contaminants. Additionally, the presence of culturable endophytes and common practice of applying beneficial microbes by cultivators renders total count tests much less effective for assessing microbial risks. Conversely, pathogen specific testing can provide much more valuable insights for cannabis user safety therefore more emphasis should be placed on targeting known risks to consumers.
References
1. Mckernan K, Spangler J, Zhang L, et al. Cannabis microbiome sequencing reveals several mycotoxic fungi native to dispensary grade Cannabis flowers. F1000Res. 2015;4:1422.
2. Mckernan K, Spangler J, Helbert Y, et al. Metagenomic analysis of medicinal samples; pathogenic bacteria, toxigenic fungi, and beneficial microbes grow in culture-based yeast and mold tests. F1000Res. 2016;5:2471.
3. Sutton S, Lum BL, Torti FM. Possible risk of invasive pulmonary aspergillosis with marijuana use during chemotherapy for small cell lung cancer. Drug intelligence & clinical pharmacy. 1986 Apr;20(4):289-91.
4. Verweij PE, Kerremans JJ, Voss A, Meis JF. Fungal contamination of tobacco and marijuana. Jama. 2000 Dec 13;284(22):2875.
5. Ruchlemer R, Amit-Kohn M, Raveh D, Hanus L. Inhaled medicinal cannabis and the immunocompromised patient. Supportive care in cancer : official journal of the Multinational Association of Supportive Care in Cancer. 2015 Mar;23(3):819-22.
6. Gargani Y, Bishop P, Denning DW. Too many mouldy joints - marijuana and chronic pulmonary aspergillosis. Mediterranean journal of hematology and infectious diseases. 2011;3(1):e2011005.
7. Bal A, Agarwal AN, Das A, Suri V, Varma SC. Chronic necrotising pulmonary aspergillosis in a marijuana addict: a new cause of amyloidosis. Pathology. 2010 Feb;42(2):197-200.
8. Szyper-Kravitz M, Lang R, Manor Y, Lahav M. Early invasive pulmonary aspergillosis in a leukemia patient linked to aspergillus contaminated marijuana smoking. Leukemia & lymphoma. 2001 Nov-Dec;42(6):1433-7.
9. Marks WH, Florence L, Lieberman J, Chapman P, Howard D, Roberts P, et al. Successfully treated invasive pulmonary aspergillosis associated with smoking marijuana in a renal transplant recipient. Transplantation. 1996 Jun 27;61(12):1771-4.
10. Llamas R, Hart DR, Schneider NS. Allergic bronchopulmonary aspergillosis associated with smoking moldy marihuana. Chest. 1978 Jun;73(6):871-2.
11. Hamadeh R, Ardehali A, Locksley RM, York MK. Fatal aspergillosis associated with smoking contaminated marijuana, in a marrow transplant recipient. Chest. 1988 Aug;94(2):432-3.
12. Chusid MJ, Gelfand JA, Nutter C, Fauci AS. Letter: Pulmonary aspergillosis, inhalation of contaminated marijuana smoke, chronic granulomatous disease. Annals of internal medicine. 1975 May;82(5):682-3.
13. Cescon DW, Page AV, Richardson S, Moore MJ, Boerner S, Gold WL. Invasive pulmonary aspergillosis associated with marijuana use in a man with colorectal cancer. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2008 May 1;26(13):2214-5.
14. Remington TL, Fuller J, Chiu I. Chronic necrotizing pulmonary aspergillosis in a patient with diabetes and marijuana use. CMAJ : Canadian Medical Association journal = journal de l'Association medicale canadienne. 2015 Nov 17;187(17):1305-8.
15. Kagen SL. Aspergillus: an inhalable contaminant of marihuana. The New England journal of medicine. 1981 Feb 19;304(8):483-4.
16. Babu TM GM, Urban MA, et al. Aspergillosis Presenting as Multiple Pulmonary Nodules in an Immunocompetent Cannabis User. Journal of Toxicology and Pharmacology. 2017;1:004.
17. Taylor DN, Wachsmuth IK, Shangkuan YH, Schmidt EV, Barrett TJ, Schrader JS, et al. Salmonellosis associated with marijuana: a multistate outbreak traced by plasmid fingerprinting. The New England journal of medicine. 1982 May 27;306(21):1249-53.
18. Chagas GM, Oliveira MA, Campello AP, Kluppel ML. Mechanism of citrinin-induced dysfunction of mitochondria. IV--Effect on Ca2+ transport. Cell Biochem Funct. 1995;13(1):53-9.
19. Shirazi-zand Z, Ahmad-molaei L, Motamedi F, Naderi N. The role of potassium BK channels in anticonvulsant effect of cannabidiol in pentylenetetrazole and maximal electroshock models of seizure in mice. Epilepsy Behav. 2013;28(1):1-7.
20. Croxatto A, Prod'hom G, Greub G. Applications of MALDI-TOF mass spectrometry in clinical diagnostic microbiology. FEMS Microbiol Rev. 2012;36(2):380-407.
21. Pham VH, Kim J. Cultivation of unculturable soil bacteria. Trends Biotechnol. 2012;30(9):475-84.
22. Spraker JE, Sanchez LM, Lowe TM, Dorrestein PC, Keller NP. Ralstonia solanacearum lipopeptide induces chlamydospore development in fungi and facilitates bacterial entry into fungal tissues. The ISME journal. 2016 Sep;10(9):2317-30.
23. Spraker JE, Jewell K, Roze LV, Scherf J, Ndagano D, Beaudry R, et al. A volatile relationship: profiling an inter-kingdom dialogue between two plant pathogens, Ralstonia Solanacearum and Aspergillus Flavus. Journal of chemical ecology. 2014 May;40(5):502-13.
24. Lucarelli C, Di Domenico EG, Toma L, Bracco D, Prignano G, Fortunati M, et al. Ralstonia mannitolilytica infections in an oncologic day ward: description of a cluster among high-risk patients. Antimicrobial resistance and infection control. 2017;6:20. PubMed PMID: 28191308.
25. Waugh JB, Granger WM, Gaggar A. Incidence, relevance and response for Ralsfonia respiratory infections. Clinical laboratory science : journal of the American Society for Medical Technology. 2010 Spring;23(2):99-106. PubMed PMID: 20499534. Pubmed Central PMCID: 4086841.
26. Coenye T, Vandamme P, LiPuma JJ. Infection by Ralstonia species in cystic fibrosis patients: identification of R. pickettii and R. mannitolilytica by polymerase chain reaction. Emerging infectious diseases. 2002 Jul;8(7):692-6.
27. Ryan D, Drysdale AJ, Lafourcade C, Pertwee RG, Platt B. Cannabidiol targets mitochondria to regulate intracellular Ca2+ levels. J Neurosci. 2009;29(7):2053-63.
28. Scott M, Rani M, Samsatly J, Charron JB, Jabaji S. Endophytes of industrial hemp (Cannabis sativa L.) cultivars: identification of culturable bacteria and fungi in leaves, petioles, and seeds. Can J Microbiol. 2018;:1-17.