By Manuel Guzmán

Manuel Guzmán is Professor of Biochemistry and Molecular Biology at Complutense University of Madrid, member of the Spanish Royal Academy of Pharmacy, and member of the Board of Directors of the International Association for Cannabinoid Medicines. His research focuses on the study of the mechanism of action and therapeutic properties of cannabinoids, especially in the nervous system. This work has given rise to more than one hundred publications in specialized international journals, as well as to several international patents on the possible therapeutic applications of cannabinoids as anticancer and neuroprotective drugs. He routinely collaborates with scientific reviewing and funding agencies.
Over the last three decades, a significant amount of knowledge has been accumulated about cannabinoids and the endocannabinoid system and, more specifically, about their possible therapeutic applications. It is obvious however that there are still many unresolved issues in this field. This article is a personal (and, therefore, subjective and rebuttable) reflection on a question that, in my view, would be crucial to understand in order to rationalise and thereby optimise the therapeutic action of cannabinoids: What is the biological function and therapeutic relevance of the endocannabinoid system in the human body?
CB1 and CB2 cannabinoid receptors are present in the human species (Homo sapiens) and also, at least, in all vertebrates and some of the invertebrates analysed so far. In fact, it is believed that these receptors arose in the evolution of animals (but not plants) a long time ago, most likely almost 600 million years ago. A first question that may arise is: Are cannabinoid receptors necessary for an organism to live? The most plausible answer is "no", since genetic engineering techniques have been used to obtain several animals lacking cannabinoid receptors in the laboratory and these animals are viable. Examples are a mammal (the mouse, Mus musculus), an amphibian (the frog Xenopus laevis), a fish (the zebrafish, Danio rerio) and a worm (the nematode Caenorhabditis elegans).
So, are cannabinoid receptors necessary for an organism to "live well"? In this case, the answer seems to be "yes". Although not necessary for life, cannabinoid receptors are necessary to maintain the correct functioning and physiological balance of an organism (what is known as "homeostasis"). In fact, the neurons and other cells of the human body produce few endocannabinoids in basal conditions of functioning, going on to generate them "on demand" when they become significantly overactivated. Thus, the endocannabinoid system is usually considered a "silent" system whose functioning is set in motion in situations in which the organism's homeostasis is altered and, therefore, whose action is aimed at restoring corporal balance when it is lost. Without the endocannabinoid system, humans could, therefore, "survive", but not "live well". In the words of Vincenzo di Marzo, the endocannabinoid system seems to have emerged in evolution to help humans to relax, feed, rest, forget (the superfluous or traumatic) and, in general, protect against numerous pathological changes.
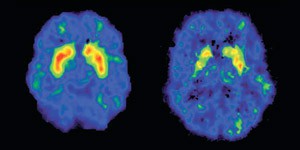
However, there is still much to learn about many precise details of how the endocannabinoid system works in the human body. For example, it is not known even in the mouse brain, let alone the human brain, in which specific places (for example, in which neuronal synapses) and by which precise mechanisms the endocannabinoids anandamide and/or 2-arachidonylglycerol are produced. Accurate analytical methods have not yet been determined to measure the minute amounts of endocannabinoids that are generated at specific synapses (this is only possible in large portions of brain necropsies), much less in real time and in the human brain. And when considering the fact that the levels of endocannabinoids rise or fall in humans in one physiological or pathological situation or another, it must be considered that these experimental determinations have been carried out in the blood plasma or, at most and on very few occasions, in the cerebrospinal fluid, but never in the precise cellular locations in which these endocannabinoids originated.
It is also important to note that the endocannabinoid system is highly ubiquitous and is expressed in many cell types throughout all the moments of human life, from the embryo to aging. The levels of its elements (cannabinoid receptors, endocannabinoids, enzymatic systems that metabolise endocannabinoids) change in very many diseases, especially in some that (a) are difficult to diagnose and treat, (b) imply comorbidity (i.e. more than one of them appears simultaneously in the same patient) and (c) are characterised by sensitisation of the central nervous system (that is, some normal physiological responses are exacerbated in such a way that the patient happens to perceive them as painful or, in general, harmful to the health). Examples of these situations include fibromyalgia, migraine, post-traumatic stress disorder, severe depression, inflammatory bowel disease and various neuropathies.
There is some evidence that cannabinoids could alleviate, at least in some patients, the symptoms associated with these diseases, perhaps enabling "normalisation" of a biological hypoactivity of the endocannabinoid system inherent in them. From my point of view however, research still sometimes moves in the field of association and not the cause-effect relationship, as well as extrapolation to large populations of patients of some preclinical evidence (read, "if it works on mice, it will work on patients") or anecdotal clinics (read, "if it seems to work on one patient, it will work on all").
In any case, this concept of "clinical endocannabinoid deficiency" (generally abbreviated as CECD, from the English clinical endocannabinoid deficiency), coined by Ethan Russo, constitutes an extraordinarily interesting challenge for future scientific-clinical research on cannabinoids. In my opinion, a "great revolution" in the medical cannabis world would come from accurately identifying a disease whose primary aetiology was the alteration of an element of the endocannabinoid system and, therefore, whose progression (and not only the palliation of its symptoms) could be attenuated by a specifically (endo) cannabinoid treatment (which, together, could be called a "cannabipathy").
Another unresolved pathophysiological question is that of the so-called "biphasic effects" of cannabinoids, already described by Raphael Mechoulam and other researchers several decades ago. For example, "low" doses of THC (and "low" in quotation marks because they vary between individuals) can decrease anxiety, inhibit vomiting, increase intake and attenuate seizures, while "high" doses of THC (again in quotation marks) can increase anxiety, induce vomiting, reduce intake and produce seizures. CBD appears to be significantly less likely than THC to produce these biphasic effects in patients, although there is evidence that it can exert them in some specific situations in mice (for example, in controlling inflammation in rheumatoid arthritis models).
What could the biphasic effects of THC be? One hypothesis, based on seminal studies carried out with mice genetically modified by the Beat Lutz and Giovanni Marsicano laboratories, proposes that "low" doses of THC would preferentially activate the CB1 receptor located in excitatory-type neurons (which produce a neurotransmitter called glutamate), while "high" doses would preferentially activate the CB1 receptor located in inhibitory type neurons (which produce a neurotransmitter called γ-aminobutyric acid, -generally abbreviated as GABA, from the English gamma-aminobutyric acid-). Obviously, both processes would produce opposite effects.
Other hypotheses propose models of differential modulation of the CB1 receptor function, depending on the dose of the cannabinoid and also on the time of exposure to the cannabinoid and the type of cannabinoid molecule under study. The future will probably provide precise answers to this complex process, which should provide a better understanding and thus improve the therapeutic action of cannabinoids.